According to medical terms, altitude sickness in the Mountains of Nepal is called Acute Mountain Sickness (AMS or altitude sickness), and it is the main difficulty that trekkers and climbers face in the high altitudes trek of Nepal. This happens when the body has difficulty coping with the decrease in oxygen levels at higher altitudes.
In Nepal, there are mountains known for their high mountains, which are the eighth Mounts over 8000 m. These are Like, Mount Everest(8,848 m.),Kanchanjangha(8,586 m.), Lhotse(8,516 m.), Makalu(8,463 m.), Cho Oyu(8,201 m.), Dhaulagiri(8,167 m.), Manaslu(8,163 m.) and Annapurna(8,091 m.) which provide trekking and climbing adventures. All this is visited by many travelers who climb up quickly without proper acclimatization. Thus, they are at higher risk of altitude sickness.
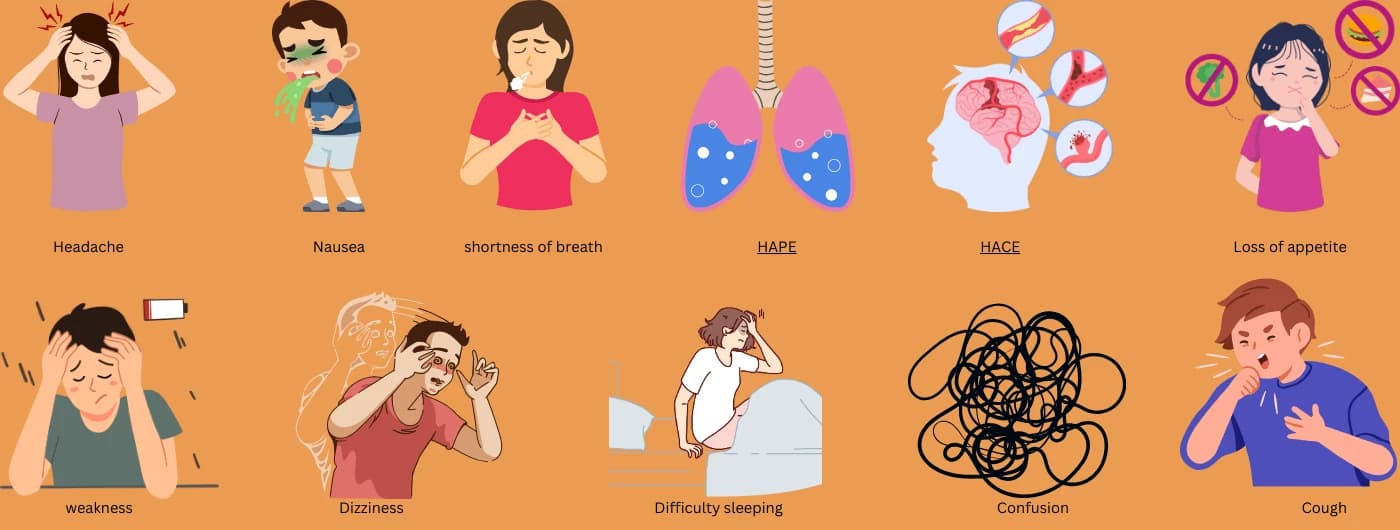
High Altitude Sickness is not selective, and anyone can be overcome by the bad symptoms even if he/she is young, fit, and a professional traveler. The symptoms develop a few hours to 24 hours after a rapid rise in altitude and include headache, nausea, suffocation, Tiredness, difficulty sleeping, and loss of appetite. If not treated, it can turn into life-threatening medical conditions such as hemorrhagic respiratory failure, High Altitude Pulmonary Edema (HAPE), or High Altitude Cerebral Edema (HACE).
Preventing Acute Mountain Sickness is all about acclimatization, thus the best way to achieve it. This can be prevented through a gradual approach where climbers take a longer time at middle altitude, and adequate water intake will minimize occurrences of the condition. Besides, trekkers are also informed to abstain from taking alcohol and relax in any strenuous activities for the first couple of days of the trek.
Most of the trekking trails in Nepal, like the Everest Base Camp Trek, Annapurna Circuit Trek, Manaslu Circuit Trek, Langtang Valley Trek, And High Altitude Trek, have provided some reserved days for acclimatization. Fascinating areas of Nepal that include mountains, and mainly the High Pass trek, Three High Pass of the Everest Region, are gorgeous but challenging for travelers. A-consciousness of a few of the signs and descending to a lower altitude whenever necessary can help in avoiding complications.
Some CMS (Chronic Mountain Sickness) recommend the trekkers to take certain medications which include acetazolamide more famously known as Diamox, they are advised to contact their guide or a travel agency like Overland Trek Nepal to seek safety precautions. Appreciation of these risks as well as preparation for them enable adventurers to visit Nepal’s famous high-altitude tourist attractions with the modest likelihood of altitude sickness in Nepal.
What is Mountain altitude sickness?
Acute Mountain Altitude Sickness, famously called altitude sickness in Nepal, is a condition that is marked by symptoms like headaches, light-headedness, and fatigue as a result of reaching a high altitude They frequently affect locations at higher altitudes such as the Everest Base Camp,Manslu Circuit or Annapurna Circuit typically above 3,500 meters (11,482 feet). and include headache, nausea, dizziness, and fatigue. Without adequate acclimatization, high-altitude sickness appears, and, in its worse forms, it can progress to HAPE or HACE.
Do you get altitude sickness in Nepal?
Of course, altitude sickness is possible in Nepal, particularly if you engage in trekking or other tourist activities at high altitudes like the Ever-popular Mount Everest Base Camp Trek or the Annapurna Circuit or Manaslu Circuit. Also referred to as Acute Mountain Sickness or AMS, this illness occurs when one moves to altitudes of 3,500 meters (11,482 feet). and more without giving the body to adjust to less oxygen concentration.
Altitude sickness manifests itself using symptoms such as headaches, nausea, dizziness, shortness of breath, and fatigue. They can develop within a few hours of attaining these altitudes and could worsen if not managed appropriately. Since the altitude increases quite steeply across Nepal, particularly in the regions of the Himalayas, adequate acclimatization has to be provided to avoid high-altitude illness.
To minimize the effect of high altitude sickness, the following measures should be taken, especially by travelers: Climbing slowly, adequate intake of water, and incorporating rest days in the climb. As obvious when climbing in the magnificent terrains of Nepal, early identification of the symptoms makes the trek much safer and more enjoyable.
How common is altitude sickness?
Altitude sickness in Nepal is very common and affects most travelers who are planning to visit high-altitude regions in Nepal. It often develops in those who climb steep slopes above two thousand five hundred meters without allowing the body to adjust to fit for trekking in the mountains which called Acute Mountain Sickness (AMS), in this condition affects alpine hikers who travel to the most famous trekking regions such as Everest Base Camp, Annapurna Circuit or Manaslu Circuit.
Research indicates that up to 50 percent of hikers and climbers who venture above 3,500 meters (11,482 feet) are likely to develop mild to moderate forms of high-altitude illness, which include headache, nausea, dizziness, and breathlessness. The possibilities are higher above 4500 meters, where risks of severe forms of AMS, including HAPE or HACE if the safety measures are not taken. Reducing the risks involves correct acclimatization, gradual ascent, adequate water intake or drinking water, and adhering to what the body is telling you.
Overland Trek Nepal is always there to help travelers make their dream trips successful without any problems when it comes to setting up the necessary preparations to handle the hurdles with altitude in the beautiful Nepalese mountains.
Symptoms of altitude sickness in Nepal Trekking
Altitude sickness, also apparent as Acute Mountain Sickness (AMS), is a standard trail that trekkers experience when journeying high-altitude trek Nepal, including Everest Base Camp, Annapurna Circuit, Manaslu Circuit, and Langtang Valley. The condition develops because oxygen concentrations are low at altitudes over 3,500 meters (11,482 feet) above sea level. It is therefore important that the signs are identified early and solve the problems to make a safe trip in Nepal and make a lifetime memorable trip for Travelers.
Common Symptoms of Altitude Sickness in Nepal
1, Mild Symptoms (Acute Mountain Sickness):
- Headache (most common and earliest sign)
- Nausea or vomiting
- Fatigue and weakness
- Loss of appetite
- Difficulty sleeping (insomnia)
- Dizziness or lightheadedness
2, Moderate Symptoms:
- Shortness of breath, even at rest
- Severe fatigue or lethargy
- Persistent headache unrelieved by painkillers
3, Severe Symptoms (High Altitude Sickness):
- Confusion or inability to think clearly
- Loss of coordination (ataxia)
- Cough-producing frothy or pink sputum (signs of High Altitude Pulmonary Edema, HAPE)
- Swelling in the brain causes severe headache, vomiting, and unconsciousness (High Altitude Cerebral Edema, HACE)
When and Where Does it Occur?
Nepal trekking altitude sickness takes place between 3000 and 5000m. Routes such as the higher altitude trips like EBC, Manaslu, and many more others, for instance, where steep patterns of climbs are likely to have been considered higher risks to trekkers who failed in the right ways to acclimatize.
How Overland Trek Nepal Ensures Your Safety
When hiking with Overland Trek Nepal, high altitude disease risks are reduced by carefully well-planned itineraries, extra days being spent on acclimatization, and guides who are well-trained to identify symptoms and treat clients. It offers the best of trekking vacations guaranteed by its tailored programs to offer a safe and fun time in the Nepalese mountains. Altitude sickness needs to be recognized early and managed appropriately so you do not ruin your trek and exacerbate your symptoms.
to be safe at any given period.
When travelers have some symptoms of High Altitude Sickness, such as Acute Mountain Sickness (AMS), it is critical to act promptly to ensure their safety. However, Here are practical steps to handle the situation at any given period.
1. Stop Ascending Immediately
- Pause your trek or travel as soon as symptoms appear. Continuing to ascend can worsen the condition and lead to severe complications like High Altitude Pulmonary Edema (HAPE) or High Altitude Cerebral Edema (HACE).
2. Descend to a Lower Altitude
- Move to a lower elevation as soon as possible, which helps to breathe easily. A descent of 300–1,000 meters can alleviate symptoms quickly.
3. Rest and Hydrate
- Rest: Allow the body time to recover. Avoid physical exertion just give rest to your body.
- Hydrate: Drink plenty of water to combat dehydration, but avoid alcohol, smoke, and caffeine.
4. Use Oxygen or a Portable Altitude Chamber (PAC)
- If available, administer supplemental oxygen or use a portable altitude chamber to simulate a lower altitude environment.
5. Take Medications
- Acetazolamide (Diamox): Helps speed up acclimatization. Take under medical supervision.
- Pain Relievers: For headaches, mild painkillers like ibuprofen or paracetamol can help.
6. Recognize Severe Symptoms
- Watch for signs of HAPE: Difficulty breathing, a persistent cough, or frothy sputum.
- Watch for signs of HACE: Severe headache, confusion, or loss of coordination.
- If these occur, descend immediately and seek emergency medical care.
7. Travel with Trained Guides
- Professional guides from companies like Overland Trek Nepal are trained to recognize and manage altitude sickness, ensuring immediate action in emergencies.
8. Emergency Evacuation
- In severe cases, arrange a helicopter evacuation to a medical facility. Always ensure you have travel insurance before you travel to Nepal that should cover high-altitude trekking, Medical, and evacuations
What are the causes of altitude sickness?
Altitude sickness, including AMS, happens when the body cannot adjust to low amounts of oxygen, common with high altitudes that stand above 3,500 meters (11,482 feet).
The condition is caused by several factors as highlighted below.
1. Rapid Ascent
- Ascending very quickly to high altitudes without enough acclimatization is the most common cause. The body struggles to adjust to the lower oxygen pressure.
2. Low Oxygen Levels
- At higher altitudes, the air pressure decreases, resulting in less oxygen available for the body to function. This imbalance can disrupt normal physiological processes.
3. Dehydration
- The dry, cold air at high altitudes, combined with increased breathing rates, can lead to dehydration, exacerbating altitude sickness symptoms.
4. Physical Exertion
- Excessive physical activity in low-oxygen environments places additional stress on the body, increasing the likelihood of developing altitude sickness.
5. Individual Susceptibility
- Some people are naturally more prone to altitude sickness due to genetic factors or pre-existing health conditions. There is no way to predict who will be affected because of this all should be serious about it.
6. Lack of Acclimatization
- If we Skip acclimatization days during the trek or climbing, it deprives the body of the opportunity to gradually adjust to lower oxygen levels.
7. Sleeping at Higher Altitudes
- When we Spend the night at a higher altitude than our body is accustomed to can make symptoms more pronounced, as the body continues to adapt while at rest.
8. Weather and Environment
- Cold temperatures, wind, and changes in barometric pressure at high-altitude places in Nepal, such as Everest Base Camp, Manaslu Base Camp, or Annapurna Circuit, can contribute to physical stress, increasing susceptibility.
These causes help trekkers ready and intervene effectively to prevent diseases like altitude illness in the beautiful but difficult mountains of Nepal.
Risk factors of altitude sickness?
Some predisposing factors may lead to the development of autism, such as treks in the mountains of Nepal. Knowledge of these risk factors enables one to be prepared in case of such incidences occasioned by travel.
1. Rapid Gain of Elevation
- Trakkers are ascending too quickly without allowing the body time to acclimatize, which is one of the most significant risk factors.
- Alpine Tropical places in Nepal like Everest Base Camp, Manaslu Base Camp, Annapurna Circuit, and other high-altitude trekking regions require gradual ascents to avoid symptoms of Acute Mountain Sickness (AMS).
2. Altitude Reached
- The risk increases at elevations normally above 3,500 meters (11,482 feet).
- Trekking to extreme heights like Everest Kala Patthar, Everest Three High Pass, Annapurna Circuit, or Manaslu Circuit involves lower oxygen levels, which can trigger high-altitude sickness.
3. Previous Altitude Sickness Experience
- If you’ve experienced altitude sickness anywhere in the world in mountainous regions before, you are more likely to develop it again.
4. Physical Condition and Fitness
- Being physically fit does not necessarily reduce the risk of altitude sickness. Both seasoned trekkers and beginners are equally susceptible if they ascend too quickly.
5. The Body Lacks sufficient water
- Inadequate fluid intake and dehydration due to increased breathing at higher altitudes can exacerbate symptoms, so we have to know how to maintain dehydration in our bodies.
6. Spending the night at High altitude
- When spending the night at higher elevations without prior acclimatization increases risk as the body continues to adjust during rest.
7. Genetic Factors
- Some people are genetically predisposed to altitude sickness, even if they follow proper acclimatization practices.
8. Excessive engagement in Physical activities
- Engaging in strenuous activities like long hikes without sufficient breaks at higher altitudes adds stress to the body.
9. Age and Health Factors
- While age is not a major factor, pre-existing medical conditions such as respiratory or cardiovascular issues can increase vulnerability.
10. Environmental Conditions
- Cold temperatures, wind, and reduced air pressure in high-altitude places in Nepal make acclimatization harder and amplify symptoms.
By recognizing these risk factors, trekkers can take proactive measures such as acclimatizing, staying hydrated, and following expert guidance from experienced trekking companies like Overland Trek Nepal to mitigate altitude sickness risks.
What are the complications of altitude sickness?
This condition is fatal if not treated or gets worse those engaging in high-altitude trek in Nepal may suffer from this sickness. These complications could escalate and become life-threatening and ought to receive early treatment.
1. High Altitude Pulmonary Edema (HAPE)
- Definition: A buildup of fluid in the lungs caused by exposure to high altitudes.
- Symptoms: Difficulty breathing, even at rest, Cough with frothy or bloody sputum, Extreme fatigue and weakness.
- Risks: HAPE can lead to respiratory failure if not treated promptly.
2. High Altitude Cerebral Edema (HACE)
- Definition: Swelling of the brain due to low oxygen levels.
- Symptoms: Severe headaches and confusion, Loss of coordination (ataxia), Hallucinations or altered mental states.
- Risks: HACE is a medical emergency and can result in coma or death if untreated.
3. Chronic Mountain Sickness (CMS)
- Definition: A long-term complication seen in individuals who live or stay at high altitudes for extended periods.
- Symptoms: Breathlessness, Fatigue and insomnia, Excessive production of red blood cells (polycythemia).
- Risks: Over time, CMS can cause heart failure or other chronic conditions.
4. Dehydration and Electrolyte Imbalance
- Causes: Increased breathing at high altitudes leads to fluid loss, and cold conditions discourage hydration.
- Symptoms: Dizziness and confusion, Muscle cramps and weakness.
- Risks: Severe dehydration can impair kidney function and exacerbate altitude sickness symptoms.
5. Hypoxia (Oxygen Deprivation)
- Definition: A condition where tissues and organs do not get enough oxygen.
- Symptoms: Bluish lips and fingertips, Rapid heart rate, and shortness of breath.
- Risks: Hypoxia can lead to organ damage, especially to the brain and heart.
6. Immune Suppression
- Effect: Prolonged exposure to high altitudes can weaken the immune system, increasing susceptibility to infections such as pneumonia.
7. Frostbite or Hypothermia (Exacerbated by Altitude)
- Risks: Low oxygen and extreme cold at high altitudes can impair the body’s ability to regulate temperature, leading to frostbite or hypothermia.
Preventing Complications
- Acclimatization: Gradual ascent and allowing time for the body to adjust.
- Descend Immediately: At the first sign of severe symptoms, move to lower altitudes.
- Medical Help: Seek professional care or arrange evacuation.
By knowing these complications, trekkers will be in a position to prepare well and minimize incidence while on high-altitude treks in the mountains of Nepal. It can be very safe if visitors hire the services of trusted companies such as Overland Trek Nepal for the treks.
How to prevent altitude sickness in Nepal?
To grasp how or why altitude sickness control is critical for adventure trekking and ultimately mountaineering in Nepal it is necessary to have a brief rendition of the reasons why altitude sickness is an important factor in trekking and mountaineering in the country. With proper preparation and care, AMS can be avoided or its severe form HAPE or HACE can be prevented in travelers.
Below are practical prevention tips:
1. Gradual Ascent
- Whenever you are Ascending, just climb slowly to allow your body time to acclimatize to maintain oxygen levels.
- Every Day, Follow the "climb high, sleep low" rule, which means climbing to a higher altitude during the day and descending to sleep.
- For high-altitude places in Nepal like Everest Base Camp or Annapurna Circuit, plan rest days between every 2-3 days of climbing.
2. Stay Hydrated
- Every day drink a minimum of 4-5 liters of water daily to prevent dehydration, a common factor in altitude sickness in Nepal.
- Avoid Smoke, alcohol, and caffeine as they can contribute to dehydration and exacerbate symptoms.
3. Acclimatization
- Allow your body time to adapt to higher elevations by including acclimatization days in your trekking itinerary whenever where you do a high-altitude trek.
- Choose destinations like Namche Bazaar on the Everest route for acclimatization hikes.
4. Medications
- Take preventive medications like Acetazolamide (Diamox) under medical supervision.
- This drug helps your body to maintain oxygen levels.
5. Pace Yourself
- Avoid overexertion during treks. Walk at a steady pace and take frequent breaks during the daytime.
- Avoid carrying heavy loads yourself if possible, or can take porters to help carry your bags.
6. Monitor Symptoms
- Be aware of early signs of high altitude sickness, such as headache, nausea, or shortness of breath.
- Stop ascending if symptoms appear, and descend if they worsen.
7. Choose a Reliable Trekking Company
- Trek with experienced guides who can monitor your health and provide immediate assistance if symptoms occur.
- Companies like Overland Trek Nepal offer well-organized itineraries and trained staff to ensure safety at high altitudes.
8. Eat a Balanced Diet
- Consume a high-calorie diet rich in carbohydrates to maintain energy levels.
- Foods like rice, pasta, and potatoes are ideal for high-altitude treks.
9. Carry Essential Gear
- Use proper trekking gear, including warm clothing, sturdy footwear, and a sleeping bag suitable for high altitudes.
- A portable oxygen canister or pulse oximeter can help in emergencies.
10. Descend to lower elevation
- Whenever possible, sleep at a lower altitude than the highest point you reach during the day.
- This practice significantly reduces the risk of AMS.
11. Travel Insurance
- Ensure you have travel insurance that covers high-altitude trekking and medical evacuation in Nepal.
By following these measures, trekkers can reduce their risk of altitude sickness and fully enjoy their journey to Nepal’s high-altitude places, such as the Everest region, Annapurna, or Manaslu Circuit. Proper preparation ensures a safer and more fulfilling adventure in the Himalayas.
Medicine for altitude sickness in Nepal
Prevention of altitude sickness is possible while carrying out high-altitude treks in the Nepalese territory for the increased success rate of the trip. Prop lore and correct utilization of drugs require medical advice, and they refrain and cure altitude sickness in Nepal.
Below are the most commonly recommended medicines and their uses:
Acetazolamide (Diamox)
1, Purpose: Prevents and treats Acute Mountain Sickness (AMS).
2, How it Works:
- Helps the body acclimatize faster by increasing breathing and oxygen levels in the blood.
- Reduces symptoms like headache, nausea, and fatigue.
3, Dosage:
- Prevention: 125-250 mg twice a day, starting 1-2 days before ascent and continuing for 48 hours at altitude.
- Treatment: The same dose can be used to alleviate mild symptoms.
Note: Requires a prescription. Side effects may include tingling in fingers and toes, increased urination, or mild dizziness.
Ibuprofen or Paracetamol
1, Purpose: Relieves mild symptoms of altitude sickness, such as headache and body aches.
2, Dosage:
- Ibuprofen: 200-400 mg every 6-8 hours as needed.
- Paracetamol: 500-1000 mg every 4-6 hours as needed.
Dexamethasone
1, Purpose: Used for severe altitude sickness symptoms or complications like High Altitude Cerebral Edema (HACE).
2, How it Works:
- A corticosteroid that reduces swelling in the brain.
3, Dosage:
- For treatment of HACE: 4-8 mg initially, followed by 4 mg every 6 hours.
- Should only be taken under medical supervision as it is not a substitute for descent.
Nifedipine
1, Purpose: Treats High Altitude Pulmonary Edema (HAPE) by reducing fluid buildup in the lungs.
2, How it Works:
- Lowers blood pressure in the pulmonary arteries, improving oxygen exchange.
3, Dosage:
- 20-30 mg every 12 hours.
Note: Used only for severe cases under medical supervision.
Oxygen Therapy
1, Purpose: Provides immediate relief in cases of severe high altitude sickness.
2, Usage:
- Supplemental oxygen can be used until descent to a safer altitude.
Ginkgo Biloba (Alternative Medicine)
1, Purpose: Some studies suggest it may help in preventing AMS.
2, Dosage:
- 120-240 mg per day, taken before the trek.
Note: Effectiveness varies, and it is not a replacement for Acetazolamide.
Important Points to Remember:
- Consult a Doctor: Always consult a physician before taking any medication for altitude sickness.
- Carry a Medical Kit: Include these medications in your trekking kit for emergencies.
- Know the Symptoms: If symptoms persist or worsen, descend immediately.
- Travel with Experts: Trekking with professionals like Overland Trek Nepal ensures proper guidance and safety.
With proper medications, trekkers can be ready to handle the effects of altitude sickness in places such as the Everest Base Camp, Annapurna Circuit, or Manaslu if they are interested, but only if the medications can be taken beforehand.
How good is it to use Diamox to prevent High altitude Sickness?
Diamox, also known as Acetazolamide is highly recommended for use when going for high altitude hiking trips, for instance, Acute Mountain Sickness. This process is carried out by raising the respiratory frequency so that the body will be in a better position to adjust to less oxygen in the altitude regions. Best when taken 1-2 days before ascent, and especially while on the climb, it can help minimize symptoms including headaches, nausea, and dizziness. Nevertheless, it does not act as a replacement for effective acclimatization as well as slow climbing up. They should also visit a physician before taking Diamox as it has some effects including tingling of the hands or feet and extended urination or slight weakness.
Are there any side effects of the altitude sickness medicine and treatment?
Some of the places include altitude sickness medications and treatments, so it is possible that the interventions can also have side effects. Some of the signs are numbness of the fingers and toes, frequent urine, dizziness, and fatigue resulting from features like Diamox (Acetazolamide). Dexamethasone may make you Serious mood or mental changes, increased hunger, or trouble sleeping. Oxygen therapy is usually harmless but can become addictive, especially if not accompanied by a decrease. However, they are advised to be taken under strict doctor supervision and should be taken as recommended by manufacturers.
Foods and Drinks for altitude sickness
Some preventative measures that can be observed when climbing is to ensure that adequate water is taken to avoid the acid in the blood since avoidance of alcohol and caffeine also leads to the accumulation of acids in the blood, thus causing Acute Mountain Sickness. In ginger or garlic tea, for example, local people often recommend them as they are helpful when it comes to soothing and improving circulation. Cereals like rice, pasta, potato, and bread contain carbohydrates that are easy on the digestive system and afford energy in high terrain. Having fruits, vegetables, and soups is important to control electrolyte levels and keep slim when adapting to climate conditions.
Helicopter Rescue in Nepal for Altitude Sickness
Helicopter rescue is essential for trekking in Nepal for those trekkers having severe altitude problems like HACE or HAPE. In remort & high altitudes such as the Everest Base Camp, Manaslu, Dopo, Kanchangangha, Dhaulagiri, Makalu, or the Annapurna Circuit as well as at high altitudes, the chopper offers fast movement to lower altitudes or hospital where right treatment is possible. This service is especially very important where a descent by foot is impossible. It is recommended that trekkers should have very good health insurance and travel insurance covering helicopter evacuation in the event of acute mountain sickness so that they can access this service cheaply and fast.
FAQs
How long will it take to feel better after treatment?
In most cases, the signs of altitude sickness subside within 24-48 hours of coming down or being given appropriate treatment like oxygen or drugs like Diamox.
Can altitude sickness be prevented?
Indeed, climbing makes slow, correct acclimatization within 2-3 days, adequate water and salt intake, non-consumption of alcohol, and being on preventive medicines such as Diamox to minimizes altitude illness.
What can I expect if I have altitude sickness?
There are different symptoms, which are general ones, such as headache, dizziness, nausea, and fatigue. If the cases are left untreated, they may lead to more severe and life-threatening situations such as HACE or HAPE.
How long does altitude sickness last?
Normal forms may clear up in 24-48 hours if the sufferer rests or descends to a lower altitude. In severe cases, the patient must seek medical assistance, and can take slightly longer to get back on course.
Is it better to have Diamox before starting a high-altitude trek?
Yes, if you visit the doctor the days before the trek and take Diamox 1-2 one- two days before the trek and during the upward movement, it will help to fight against altitude sickness. It is advisable to consult your doctor on when and how to take the drugs.
What is Diamox, and how can we use it?
Diamox contains Acetazolamide, and it is employed for avoiding and treating high-altitude illnesses. It has the effect of raising breathing and the level of oxygen in the blood. This is taken as directed, usually 125-250 mg twice a daily.
How do I take care of myself if I feel I have symptoms of altitude sickness?
Lie down, no more climbing, drink plenty of water, and Stick to medications recommended by the doctor. In the case where the symptoms get worse, you should go to a lower altitude and look for a doctor.
How serious is altitude sickness?
Altitude sickness can be in lesser and more severe forms; altitude sickness is one that varies in terms of palpability. Mild cases have mild manifestations, and while severe cases of HACE or HAPE may have serious complications including fatalities, patients need to descend and receive treatment.
How much does a helicopter rescue in Nepal cost for altitude sickness?
The helicopter rescue cost in Nepal also differs with the area, and it starts from 2,500 dollars to 8,000 dollars. The authors strongly advise taking out extensive travel health insurance that includes medical repatriation.